The Science of Exosomes in Skincare: Evidence, Sources, and Regulatory Reality in 2025
Exosomes offer intriguing anti-aging skincare potential, but with no FDA-approved products in 2025, efficacy and safety remain under investigation, especially for human-derived sources.
Exosomes represent one of the most scientifically intriguing yet controversial developments in modern skincare. These microscopic cellular messengers promise revolutionary anti-aging benefits, but their journey from laboratory bench to beauty shelf is fraught with regulatory complexities, ethical debates, and scientific uncertainties. With no FDA-approved exosome products for cosmetic use as of 2025, consumers and professionals alike are navigating an increasingly complex landscape of claims, evidence, and safety considerations.
Comparison of exosomes, growth factors, and peptides molecular structures
Understanding Exosomes: The Cellular Communication Revolution
What Are Exosomes Exactly?
Exosomes are extracellular vesicles measuring 30-150 nanometers that function as sophisticated biological messengers between cells. Unlike simple skincare ingredients, exosomes carry complex cargo including proteins, lipids, microRNAs, and growth factors that can potentially reprogram cellular behavior. This unique mechanism of action sets them apart from traditional skincare actives by working at the cellular communication level rather than merely providing surface benefits.[1][2][3][4]
The International Society for Extracellular Vesicles (ISEV) defines exosomes as specific types of extracellular vesicles formed through the endosomal pathway. They're naturally secreted by virtually all cell types and play crucial roles in physiological processes including immune regulation, tissue repair, and cellular homeostasis.[2][3][1]
The Mechanism: How Exosomes Theoretically Transform Skin
Exosomes work through several interconnected pathways that make them particularly compelling for skin applications:[1][3]
Cellular Reprogramming: Exosomal cargo can alter gene expression in target cells, potentially "instructing" aged skin cells to behave more youthfully.[4]
Growth Factor Delivery: They transport multiple growth factors simultaneously, including TGF-β, VEGF, FGF, and PDGF, which regulate collagen production and tissue regeneration.[2][1]
Anti-Inflammatory Action: Exosomal miRNAs like miR-146a help reduce inflammatory cytokines and promote tissue repair.[3]
Enhanced Penetration: Their lipid bilayer structure allows deeper skin penetration compared to traditional topical actives.[4]
Sourcing Methods: From Cells to Cosmetics
Human-Derived Sources and Their Complexity
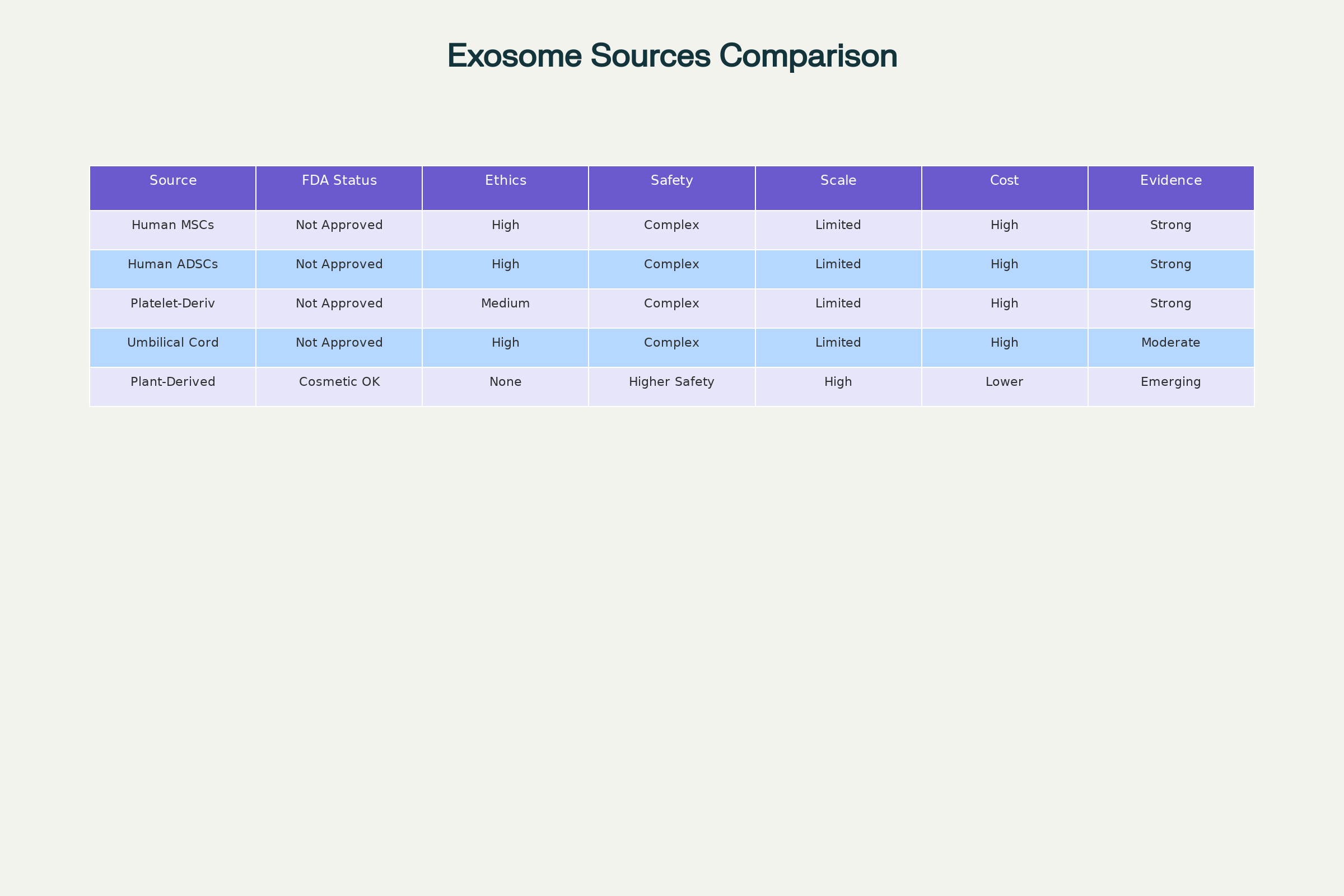
Comparison of different exosome sources for skincare applications in 2025
Mesenchymal Stem Cells (MSCs) represent the most studied source for therapeutic exosomes. These can be derived from multiple tissues:[1][3]
- Adipose tissue: Relatively accessible through liposuction procedures, producing exosomes rich in regenerative factors[5][6]
- Bone marrow: More challenging to obtain but historically the gold standard for MSC research[1]
- Umbilical cord tissue: Collected from donated umbilical cords after birth with maternal consent, offering high potency[7][8]
Platelet-derived exosomes have shown particular promise in clinical studies. Platelets naturally respond to tissue injury by releasing growth factors, making platelet-derived exosomes theoretically ideal for skin repair applications.[9][10][11]
Extraction and Purification Challenges
The isolation process significantly impacts exosome quality and therapeutic potential. Current methods include:[12][13]
Ultracentrifugation: Considered the gold standard but time-intensive and potentially damaging to exosome integrity.[13][12]
Size-Exclusion Chromatography: Preserves bioactivity but cannot separate exosomes from similarly-sized particles.[12]
Immunoaffinity Capture: Highly specific but limited by available surface markers.[13]
Commercial Precipitation Kits: Faster but often co-isolate non-exosomal particles, reducing purity.[12][13]
The Plant-Derived Alternative
Plant-derived exosome-like nanovesicles (PDENs) are emerging as a safer, more sustainable alternative. These vesicles from sources like cabbage, ginger, and roses offer several advantages:[14][15][16]
- No ethical concerns regarding human tissue use
- Lower immunogenicity risk due to evolutionary distance
- Easier large-scale production and standardization
- Reduced regulatory complexity for cosmetic applications
However, critics argue that plant exosomes may be less bioactive for human skin due to species-specific differences in cellular communication pathways.[17]
Clinical Evidence: What the Research Actually Shows
Comprehensive Analysis of Human Studies
A systematic review of clinical trials reveals 12 published studies examining exosomes in dermatological applications, with a total of 298 participants across various skin concerns.[18]
Anti-Aging Applications (6 studies, 265 participants):
The Proffer et al. 2022 study represents the largest investigation to date, involving 56 participants using platelet-derived exosome serum twice daily for six weeks. Results showed a mean improvement in skin health score of 224.2 ± 112.8 (p ≤ 0.0001), with top responders achieving a 440% increase in multiple skin parameters.[10]
Park and Kwon 2023 conducted the most rigorous split-face trial, combining exosomes with microneedling. Their 28 participants showed statistically significant improvements in wrinkle reduction (12.4% vs 6.6% control), skin elasticity (+11.3% vs -3.3% control), and melanin reduction (9.9% vs 1.0% control).[19]
Acne Scar Treatment (1 study, 25 participants):
Kwon et al. demonstrated that adipose stem cell-derived exosomes combined with fractional CO₂ laser therapy achieved a 32.5% reduction in ECCA scores compared to 19.9% with laser alone (p < 0.01). Notably, treated areas also showed shorter recovery time and reduced post-procedural erythema.[20]
Alopecia Treatment (1 study, 30 participants):
Ersan et al. reported significant increases in hair density from 149.7 ± 13.7 hairs/cm² at baseline to 157 ± 18.3 hairs/cm² at 12 weeks (p = 0.002) using foreskin-derived MSC exosomes.[21]
Evidence Quality Assessment
While results appear promising, significant methodological limitations affect evidence interpretation:[18]
- Small sample sizes: Average 37 participants per study
- Short duration: Most studies lasted 4-12 weeks
- Limited diversity: Predominantly female participants of specific ethnic backgrounds
- Lack of standardization: Varying exosome concentrations, sources, and application methods
- Publication bias: No negative results published to date
Exosomes vs. Growth Factors vs. Peptides: The Comparative Reality
Mechanism of Action Differences
Peptides function as targeted signalers that can stimulate specific cellular responses like collagen production. They're well-characterized, stable, and have decades of safety data in cosmetic applications.[22][23]
Growth Factors are individual protein molecules that bind to specific cellular receptors to trigger particular biological responses. They're more potent than peptides but face stability challenges and potential safety concerns with prolonged use.[24][25]
Exosomes represent a multi-factorial approach, carrying dozens of bioactive molecules simultaneously. This complexity could theoretically provide superior results but also makes them harder to standardize and predict.[1][3][26]
Clinical Efficacy Comparison
Peptides: Extensive clinical data supporting modest but consistent improvements in skin hydration, firmness, and fine lines over 8-12 weeks of use.[22][23]
Growth Factors: Strong evidence for wound healing and post-procedural recovery, with some data supporting anti-aging benefits.[24][25]
Exosomes: Limited but promising data showing potentially superior results, but with significant methodological limitations and no head-to-head comparisons.[18]
Safety Profile Analysis
Peptides: Excellent safety record with minimal allergic reactions and no systemic absorption concerns.[22][23]
Growth Factors: Generally safe topically but concerns about cellular overstimulation with long-term use.[24]
Exosomes: Unknown long-term safety profile due to limited clinical exposure and complex, variable composition.[26]
Regulatory Landscape: The FDA Reality Check
Current Regulatory Status
No exosome products have FDA approval for any cosmetic or therapeutic skin application as of 2025. The FDA has issued multiple warnings regarding exosome products, emphasizing that:[27][28]
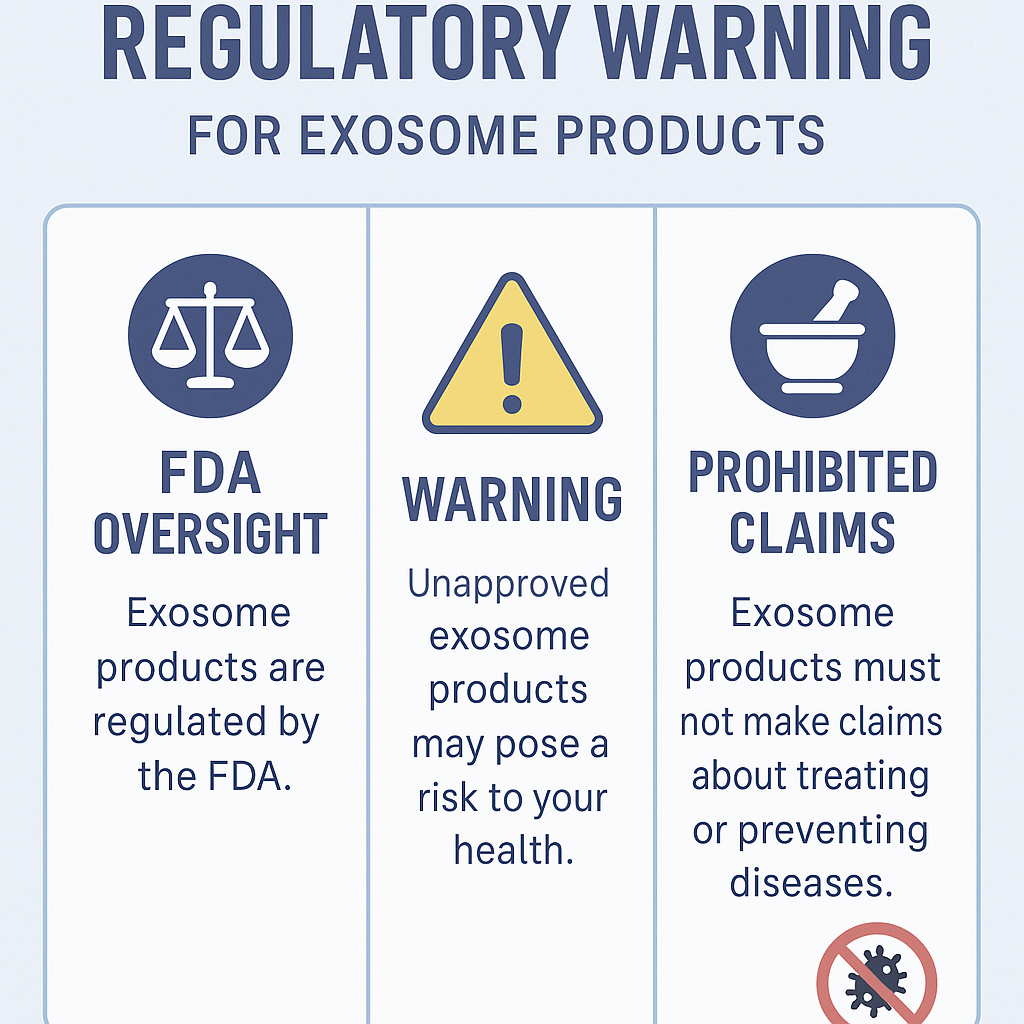
FDA regulatory status and warnings for exosome products in skincare
- All therapeutic claims require FDA approval through the biologics license application (BLA) process
- Human-derived exosomes are considered biological products subject to strict regulatory oversight
- Current marketing practices often violate FDA regulations regarding unapproved medical devices
Recent FDA Enforcement Actions
The FDA issued warning letters to multiple companies in 2024-2025 for marketing unapproved exosome products. Supreme Rejuvenation LLC received a warning letter in May 2025 for selling "100 Billion Exosomes: Human Umbilical Cord Mesenchymal Stem Cell Derived Exosomes" with therapeutic claims.[28][29]
Key FDA positions include:[27][28]
- No approved exosome products for COVID-19, orthopedic conditions, neurological disorders, or cardiovascular diseases
- Cosmetic products cannot make drug claims about treating or preventing diseases
- Safety data requirements remain unfulfilled for most commercial exosome products
International Regulatory Variations
European Union: Similar restrictions on therapeutic claims, with additional concerns about novel food regulations for orally consumed plant exosomes.[30]
Asian Markets: More permissive approaches in some jurisdictions, but increasing scrutiny as safety questions emerge.[31]
Safety Considerations and Ethical Concerns
Human-Derived Exosome Safety Issues
Immunogenicity Risks: Human-derived exosomes may trigger immune responses, particularly with repeated use.[26][32]
Contamination Potential: Risk of viral, bacterial, or prion transmission from human tissue sources.[32]
Batch Variability: Donor-to-donor differences in exosome composition create consistency challenges.[33]
Unknown Long-term Effects: No studies examining safety beyond 12 weeks of use.[18]
Ethical Sourcing Concerns
Umbilical Cord Tissue: While obtained with maternal consent, questions remain about commodification of birth tissues and equitable access to therapies.[34][35]
Fetal Tissue Misconceptions: Despite claims otherwise, some products may utilize ethically questionable tissue sources.[34]
Informed Consent: Current consent processes may not adequately address future commercial uses of donated tissues.[35]
Plant-Derived Safety Profile
Plant-derived exosomes offer improved safety profiles with lower immunogenicity risk and no human tissue ethical concerns. However, challenges include:[14][15]
- Limited efficacy data compared to human-derived sources
- Potential allergenicity from plant proteins
- Regulatory uncertainty regarding novel botanical extracts
Clinical Evidence Summary
Our analysis reveals cautious optimism supported by preliminary evidence but tempered by significant limitations:
Strengths:
- Consistent positive outcomes across diverse applications
- Low reported adverse event rates in clinical trials
- Promising mechanistic rationale for skin applications
- Multiple independent research groups reporting similar findings
Limitations:
- Small study populations limiting statistical power
- Lack of standardization across products and protocols
- No long-term safety data beyond 12 weeks
- Publication bias favoring positive results
- Minimal regulatory oversight of commercial products
Future Directions and Recommendations
Research Priorities
Large-scale randomized controlled trials with standardized protocols, diverse populations, and longer follow-up periods are essential.[18]
Standardization efforts must address exosome characterization, dosing protocols, and quality control measures.[33]
Mechanistic studies should elucidate how different exosome sources and compositions affect specific skin parameters.[26]
Clinical Practice Considerations
Professional treatments utilizing exosomes should be limited to licensed medical settings with appropriate informed consent and safety monitoring.
At-home products should be approached with caution, prioritizing plant-derived sources until human safety data improves.
Patient education must address the experimental nature of exosome therapies and realistic outcome expectations.
Conclusion: Navigating the Promise and Reality
Exosomes in skincare represent a scientifically fascinating frontier with genuine therapeutic potential, but current evidence remains insufficient to support widespread adoption. The absence of FDA approval, limited long-term safety data, and regulatory uncertainties require careful consideration by both professionals and consumers.
Plant-derived alternatives may offer the most promising near-term path forward, providing improved safety profiles while regulatory frameworks develop. However, the skincare community must resist the temptation to oversell benefits and instead focus on rigorous scientific validation.
For millennial women seeking science-based skincare solutions, exosomes may eventually prove transformative, but current evidence suggests maintaining realistic expectations while supporting continued research into this promising but complex technology.
Sources
- Revolutionizing dermatology: harnessing mesenchymal stem/stromal cells and exosomes in 3D platform for skin regeneration
- Exosomes derived stem cells as a modern therapeutic approach for skin rejuvenation and hair regrowth
- Effectiveness of Extracellular Vesicle Application in Skin Aging Treatment and Regeneration: Do We Have Enough Evidence from Clinical Trials?
- Regenerative topical skincare: stem cells and exosomes
- hMSC exosomes as a novel treatment for female sensitive skin: An in vivo study
- Efficacy of combined treatment with human adipose tissue stem cell‐derived exosome‐containing solution and microneedling for facial skin aging: A 12‐week prospective, randomized, split‐face study
- Topical Wharton's Jelly MSC‐Derived Age Zero™ Exosome Treatments After Micro‐Needling for Skin Rejuvenation
- Exosomes derived from umbilical cord mesenchymal stem cells ...
- The Innovative and Evolving Landscape of Topical Exosome and Peptide Therapies: A Systematic Review of the Available Literature
- Tapping into the potential of platelet-derived exosomes in aesthetics
- Cardioprotection by cardiac progenitor cell-secreted exosomes: role of pregnancy-associated plasma protein-A
- Conventional and Nonconventional Sources of Exosomes–Isolation ...
- Clinical applications of stem cell-derived exosomes - Nature
- Plant‐derived exosomes: A Green Nanomedicine for Cancer
- Recent Advances in the Isolation Strategies of Plant-Derived Exosomes and Their Therapeutic Applications
- A New Therapeutic Approach With Rose Stem-Cell-Derived Exosomes and Non-Thermal Microneedling for the Treatment of Facial Pigmentation
- Plant-Derived Exosome-Like Nanovesicles: Current Progress and Prospects
- Effectiveness of Extracellular Vesicle Application in Skin Aging Treatment and Regeneration: Do We Have Enough Evidence from Clinical Trials?
- Efficacy of combined treatment with human adipose tissue stem cell‐derived exosome‐containing solution and microneedling for facial skin aging: A 12‐week prospective, randomized, split‐face study
- Global trends in the clinical utilization of exosomes in dermatology: a bibliometric analysis
- Exosomes: A Comprehensive Review for the Practicing Dermatologist
- Safety Assessment of Plant-Derived Proteins and Peptides as Used in Cosmetics
- An efficient mRNA display protocol yields potent bicyclic peptide inhibitors for FGFR3c: outperforming linear and monocyclic formats in affinity and stability
- Exosomes \& Growth Factors: Advanced Skin Rejuvenation - PSH
- Growth Factors vs Exosomes: What's the Difference? - SOM Aesthetics
- Exosomes in skincare: Everything You Need To Know
- Consumer Alert on Regenerative Medicine Products Including Stem ...
- Why exosomes are an exciting breakthrough in skincare | ASPS
- Supreme Rejuvenation, LLC - 700749 - 05/05/2025 - FDA
- Exosomes in skin care: Promise and challenges revealed in new study
- The Rise of Exosome-Based Cosmeceuticals in 2025 - BioInformant
- Exosomes in Skincare: Are They Worth the Hype?
- Exosome Source Matters: A Comprehensive Review from the ...
- What are Some Ethical Issues with Exosome Therapy? - Advancells
- Stem Cell Research Controversy: Ethics, Science, and Society (2024)